Care partners1are vital members of a patient's care team across a wide variety of conditions, providing invaluable support both inside and outside formal healthcare settings. To better understand the care partner experience, needs, and preferences, IQVIA conducted a survey with 200 care partners of patients across three broad therapeutic areas: oncology (n=75 care partners), progressive cognitive disease (n=75 care partners), and mental health disorders (e.g., bi-polar, schizophrenia, OCD, PTSD, depression; n=50 care partners). Findings from this survey have been analyzed and presented here to enhance our understanding of care partner characteristics and needs. Additionally, we examine the current support provided by pharmaceutical companies for care partners and explore ways in which this support can be enhanced in the future.
Care partners are often family members such as parents (31% in our survey), adult children (24%), and spouses (21%), but they can also include friends (6%), and even paid providers.2 In addition, care partners tend to be female, with 59% of surveyed care partners identifying as women.2 Care partners are evident in a wide variety of therapeutic areas, but they may be most important for patients with chronic or terminal diseases (e.g., cancer), progressive cognitive disorders (e.g., dementia and Alzheimer's disease), diseases that cause mobility issues (e.g., stroke, neurological disorders such as multiple sclerosis and Parkinson's disease), mental health conditions (e.g., depression, anxiety, bipolar disorder, schizophrenia), and for pediatric patients. Care partners’ proximity to the patient can provide physicians with knowledge of the patient's routine and history. Additionally, they can provide support to the patient both when they are receiving medical care in a hospital or physician’s office, and at home or during activities of daily living. As a result, the role of a care partner is broad and can include:
- Logistical support (71% of care partners surveyed provide significant logistical support)2: Scheduling appointments, managing care teams, providing transportation, navigating legal matters, supporting activities of daily living (e.g., housekeeping, meal preparation), etc.
- Emotional support (77% of care partners surveyed provide significant emotional support)2: Providing empathy and encouragement, physical presence, educating and interacting with family members and friends, learning about disease and treatment options, advocating for the patient, etc.
- Medical support (69% of care partners surveyed provide significant medical support)2: Making sure the patient takes their medication, helping administer medication, monitoring side effects, providing thoughts on treatment decisions, discussing medical needs with the care team, researching the patient’s diagnosis and treatments.
- Financial support (60% of care partners surveyed provide significant financial support)2: Providing direct monetary coverage and/or insurance, navigating insurance and payment requirements, exploring benefits, filling out paperwork (e.g., tax documents, applications for assistance programs), providing access to traditional financial support options (i.e., co-pay support), etc.3
While they may have a close relationship to the patient, a care partner’s needs are distinct from patient needs, with 30% of care partners surveyed expressing that their needs are extremely different from the needs of the person for whom they provide care.2 A care partner's burdens are often closely tied to the patient’s journey, but their lived experience can vary in subtle, yet impactful ways. For example, a patient may be struggling emotionally with the knowledge that they have a very serious illness, while the care partner is more occupied with communicating the prognosis to family members and loved ones. Or a patient may be dealing with the emotional and financial challenges of early retirement due to their disease, while their spouse care partner struggles with the transition of becoming the sole breadwinner and primary provider of health insurance.
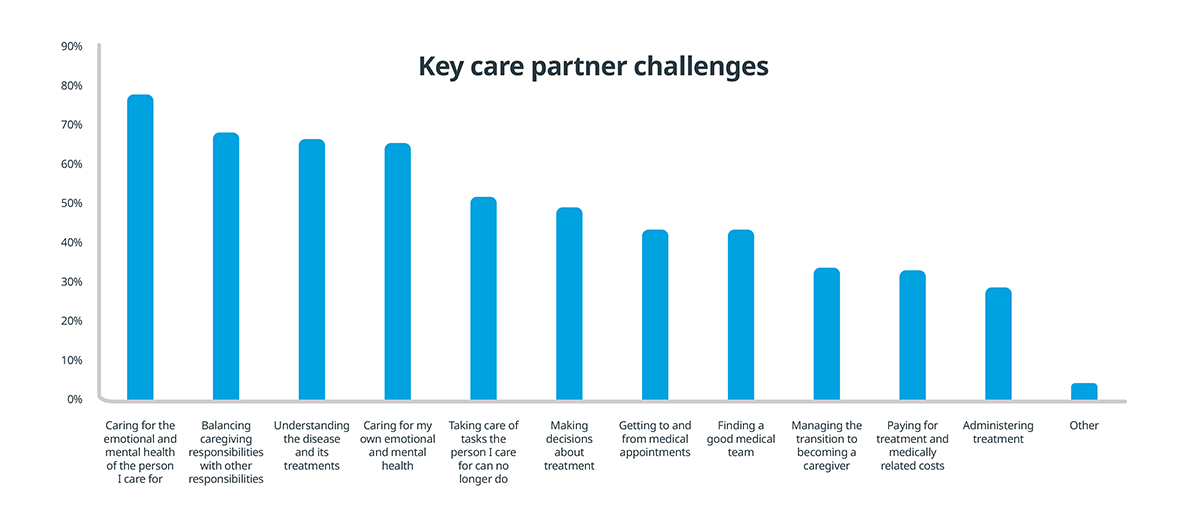
Care partners surveyed indicated that emotional and mental health challenges are some of the greatest challenges they face, both tending to the emotional/mental health needs of the person they care for as well as their own. The challenges associated with balancing responsibilities also rise to the top in terms of juggling caregiving responsibilities in addition to other responsibilities, and taking care of tasks the person they care for can no longer do themselves. Finally, understanding the disease and its treatments is also a key challenge for care partners.2 Together these challenges indicate the significant emotional, logistical, and educational needs of care partners.
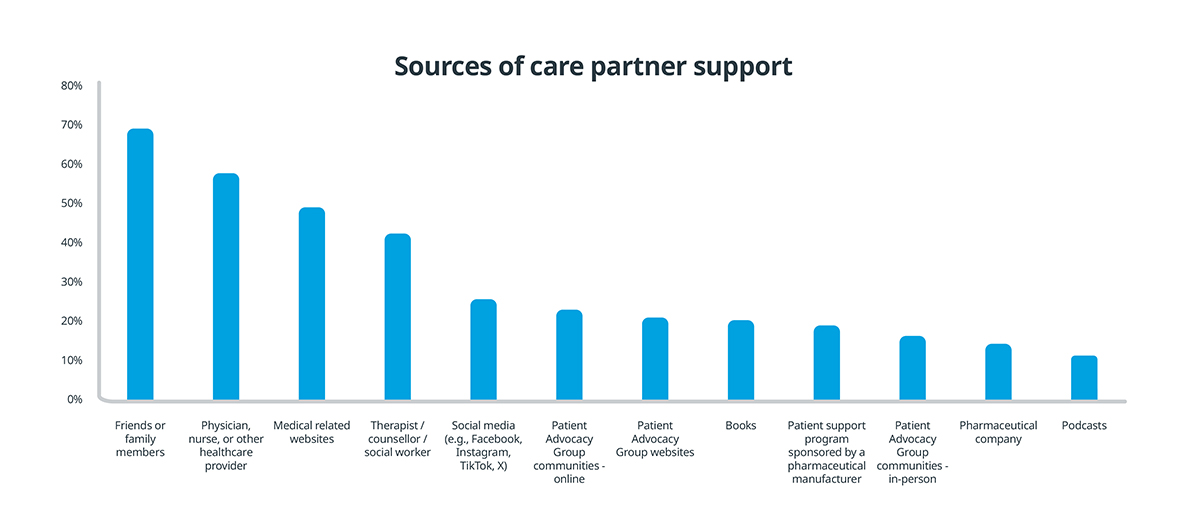
Despite the challenges they face, the care partner’s role is often overlooked. Care partners tend to operate in the background, and their efforts and experiences may be overshadowed by what the patient is experiencing. At present, the vast majority of care partners receive support from personal sources, with 69% of care partners stating they rely on friends and family for support.2 Merely 15% of care partners indicated that they relied on a pharmaceutical company for support.2 This is likely due in part to the fact that pharmaceutical investment in support services has largely targeted patients, not their care partners. In 2021, pharmaceutical companies spent over $5 billion on patient support programs.4 These programs offer patients critical support in financial assistance, support group connections, disease awareness, and information on how to use medications or devices.2 In comparison, dedicated care partner support is lacking, with most support services supplementing the already-existing patient support service. Indeed, IQVIA’s survey indicated that while 32% of care partners had utilized support services provided by pharmaceutical companies, only 37% of those (12% of overall care partners) stated the support was meant specifically for them as a care partner.2 While this is understandable, given the lack of focus on care partners, it can still be to the detriment of care partners themselves, contributing to feelings of isolation and a lack of resources.
Intentional investment in supporting care partners can enhance the well-being of both care partners and patients. Support targeted at the care partner – whether logistical, emotional, or financial – can help reduce the burden of the role and empower them to better care for the patient. For example, when a care partner has access to a support group through which they can specifically connect with other care partners, they can share experiences and receive emotional support that might not otherwise be available to them. A supported care partner can more easily help manage the patient's condition, facilitate care coordination, and ultimately promote adherence. This has the potential to improve patient well-being, with the additional benefit of reducing healthcare costs in the long run by preventing avoidable hospitalization and complications.
However, there are many challenges to developing and executing care partner support. Just like patients, care partners cannot be approached with a “one-size-fits-all” mindset. Various factors such as age, gender, technological proficiency, and geographic location can influence whether care partners are inclined to seek or accept support for their caregiving roles. In addition, with limited resources and a focus on patients first, care partner support may struggle to receive the funding and attention it needs. Considering that care partners’ needs are greatest when the patient need is also greatest2, pharmaceutical companies should consider overlaying their existing patient support programs with similarly timed care partner support.
Considering the benefits and challenges of supporting care partners, IQVIA recommends that industry focus its efforts on:
- Mental health and psychological support: Care partners experience significant social isolation and emotional challenges. Nearly three quarters of care partners indicate that emotional and mental health is a significant challenge for them and the person they care for.2 Industry should focus on identifying and supporting existing care partner support networks, and providing resources to develop new ones where they are unavailable.
- Logistical and financial support: Care partners can struggle with changing financial priorities as their household needs change and they have to financially support the patient. These financial struggles are only exacerbated by increased logistical costs as the patient manages their disease and treatment (i.e., frequent travel to the doctor for appointments, or needing an overnight stay at the treatment hospital). Nearly 50% of care partners highlighted needing help with getting to and from appointments, and over 30% said that they need help with paying for treatment and medical costs.2 Identifying impactful ways to financially support care partners, directly or indirectly, is an important part of holistically supporting care partners and their patients.
- Education and skill development: Care partners, like patients, are often not educated about their disease and treatment, especially at diagnosis. 67% of care partners stated that they struggled with understanding the disease and its treatment, and nearly half of them felt that they struggled to get a good medical team to support them.2 By providing educational resources specifically targeted to care partners, industry can address these challenges.
Initiatives aimed at supporting care partners should not operate in isolation, but rather in conjunction with existing support structures such as patient advocacy groups and support group networks. Collaboration and partnership between industry, existing community groups, and other key stakeholders in the healthcare system is vital to not only create impactful support, but also conserve resources and ensure cost-effective operations.
Investing in care partners is not an inexpensive proposition, but there is high value in supporting these vital members of the care team. And as the industry strives towards a more patient-centric care model, care partners are an integral part of that transition due to their involvement in care. Industry should focus on providing educational, financial, and logistical support. IQVIA is ready to leverage our data and expertise to support these efforts and provide key strategic insights to improve patient and care partner outcomes.
References:
- We use the term "care partner" instead of "caregiver" to promote greater inclusivity and respect in our language. We believe the term "care partner" underscores the collaborative nature of the relationship between the patient and the care partner, while also mitigating the power imbalance that can be implied when one person is solely seen as a caregiver. Additionally, using the term "care partner" may contribute to reducing any stigma associated with dependency often associated with the concept of needing a caregiver.
- Survey of 200 care partners (n=75 oncology care partners, n=75 progressive cognitive disease care partners, n=50 mental health care partners) conducted by IQVIA in November, 2023. Significant support defined as a rating of 6 or 7 on a 7 point Likert scale, where 1 is no contribution and 7 is significant contribution.
- A larger proportion of non-white care partners provide significant financial support when compared to white care partners (70% vs. 50% respectively)
- https://www.fiercepharma.com/marketing/pharmas-return-5-billion-spent-yearly-patient-support-programs-only-3-use-survey.
Related solutions
Deploy sales representatives, clinical nurse educators, field reimbursement specialists virtually or in the field to communicate the benefits of your therapy.
Grow your brand, now and through patent expiry
Flexible solutions. Responsive teams. Data-driven insights.

















