IQVIA is working to advance public health in partnership with other companies, governments, and non-governmental organizations, from fighting opioid addiction to addressing antibiotic resistance.












Discussions in New York in the context of the UN General Assembly High-Level Meeting on Antimicrobial Resistance (AMR) showed the interest and determination of many stakeholders in finding solutions to this issue, stressing the need for progress in areas such as sustainable funding, diagnostics, research and development, prevention tools, clinical practice, national guidelines and policies, partnership platforms, and healthcare system infrastructure. These exchanges also highlighted the need for collecting high-quality data to determine the magnitude of the problem and serve as a common denominator in the generation of novel solutions.
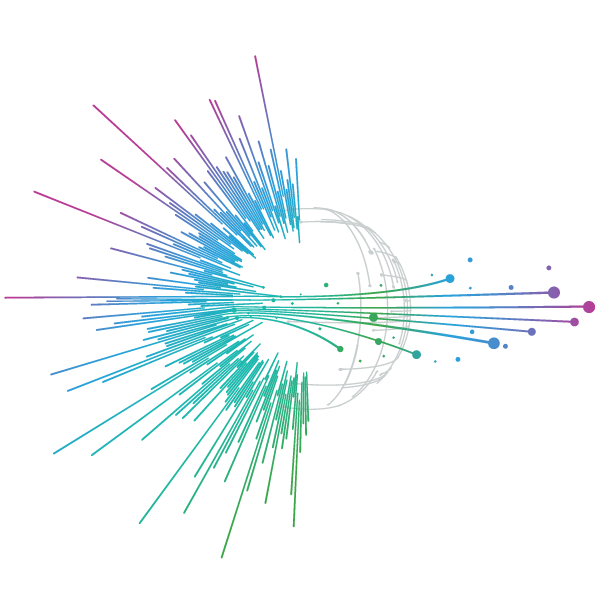
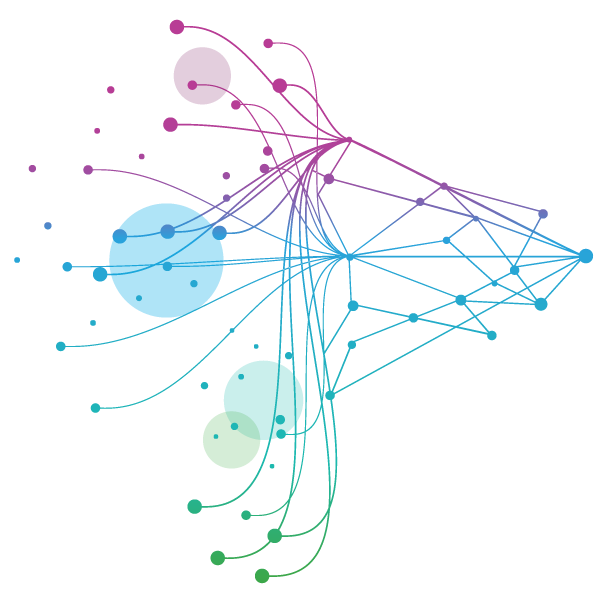
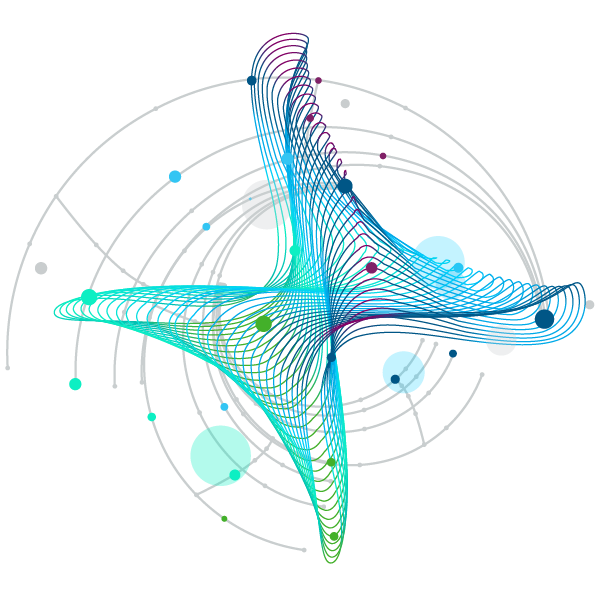
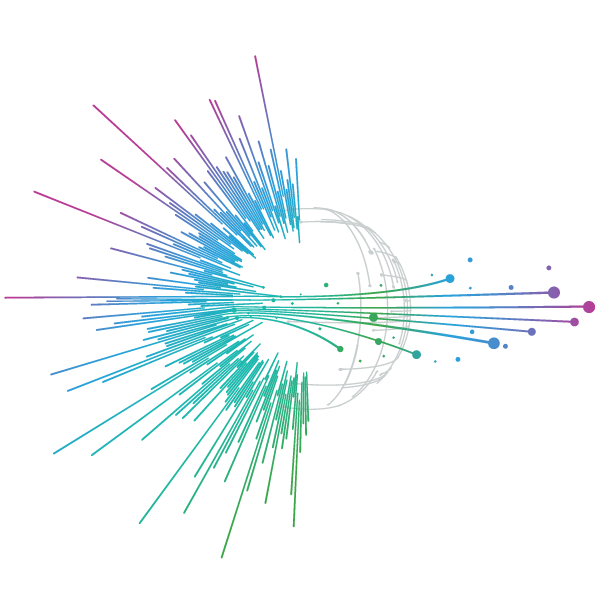
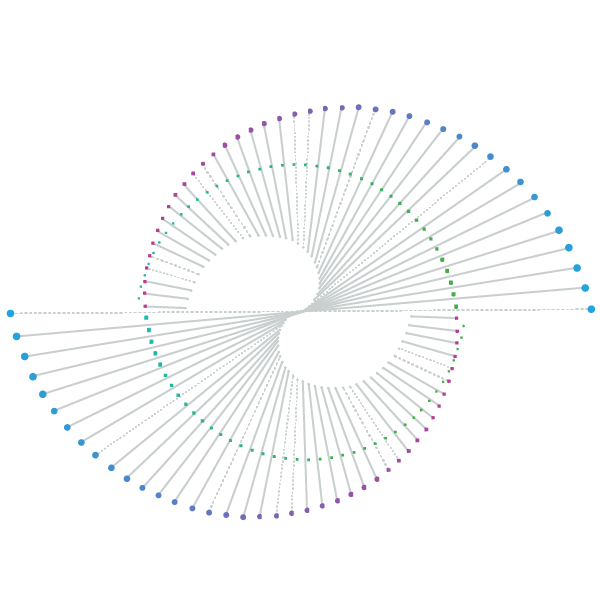
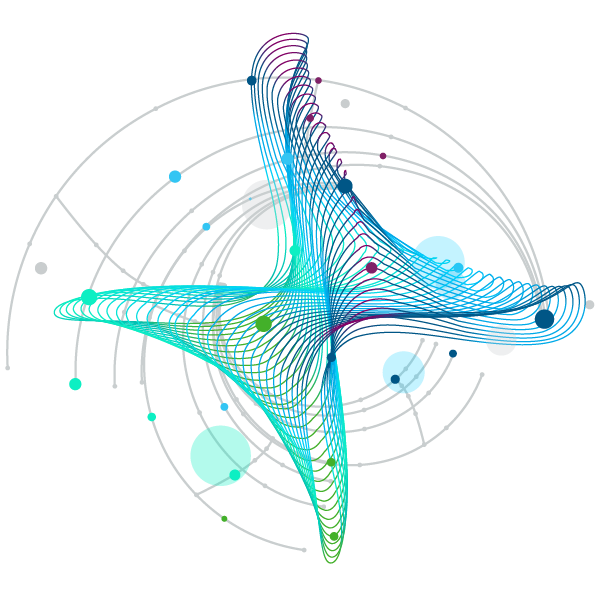
To contribute to this debate, IQVIA hosted a side event on 25 September to share its latest thinking on the role of data in informing actions to curb the impact of AMR. The event opened with the launch of a white paper1 examining the central importance of national antibiotic assessment reports as tools to guide antibiotic policies and, as a result, optimize the use of and access to these medicines. A collaborative effort between IQVIA, City St. George’s University of London and the University of Oxford, the paper’s findings show the increased use of Access, Watch and Reserve (AWaRe) representative antibiotics globally (figure 1) and gaps in AMR national action plans (NAPs) in enabling more comprehensive policy-based approaches (figure 2).
Figure 1. Regional antibiotic use across three AWaRe representative drug classes from 2013 to 2023 (in defined daily doses per 1,000 inhabitants per day)
Source: IQVIA EMEA Thought Leadership based on analysis of IQVIA MIDAS data and World Bank development indicators
Figure 2. References to national antibiotic policies in available NAPs (as of August 2024)
Source: IQVIA EMEA Thought Leadership analysis based on WHO’s library of AMR NAPs
After the presentation of the paper, Dr. Rachel Freeman, Principal in IQVIA’s Global Public Health practice, facilitated a panel comprised of global experts and practitioners, including Prof. Mike Sharland, Professor of Pediatric Infectious Diseases, City St. George’s University of London; Dr. Thomas Breuer, Chief Global Health Officer at GSK; Prof. Mirfin Mpundu, Senior Technical Advisor for AMR and Biodefense at USAID; and Prof. Kevin Outterson, Executive Director of CARB-X. World Health Organization (WHO) attendees contributed with additional points of view. This conversation reflected on the actions needed to improve the AMR response from a data and partnerships perspective.
In panel: [From left to right] Prof. Mike Sharland, City St. George’s University of London; Dr. Thomas Breuer, GSK; Prof. Mirfin Mpundu, USAID; Dr. Kevin Outterson, CARB-X; and Dr. Rachel Freeman, IQVIA Global Public Health. Presenting for IQVIA [From left to right]: David Franks, Vice-President, Global Public Health, and Daniel Mora-Brito, Engagement Manager, Global Public Health, EMEA Thought Leadership.
What did we learn?
"Thinking about where we are now is like going into the glass section of a jewelry store being tasked with killing a dangerous insect that is flying around the premises. If they blindfold you and give you a baseball bat to go after the insect, you will destroy valuable things and probably be ineffective. This is how combatting AMR without data looks like."
Kevin Outterson, Executive Director, CARB-X
The panel resulted in several lessons and points of view:
- The data on antibiotic use exists, but it is insufficient, scattered, and may lack quality:
There are multiple data sources to understand antibiotic use, but they are rarely standardized, properly integrated within interoperable systems, or validated by international authorities. Data ‘blind spots’ are present in many countries but are particularly prominent in low- and middle-income geographies. Looking beyond large-scale surveys in hospitals and delving into, for instance, private care settings and national antibiotic use, requires new methodological approaches. WHO is proposing the formation of a global data collaborative with a solid set of indicators that can be subject to comparisons and real-world validation exercises, increase the quality of inputs, and set accountability frameworks. -
Integrating population health data and other sources into the analysis of antibiotic use can help decision-makers understand the issue better:
Achieving a more responsible use of antibiotics demands greater engagement from countries in understanding what types of infections need to be treated and determining the level of access required for relevant anti-infectives. This calls for the incorporation of population health data into national assessments to paint a more accurate picture of antibiotic use and access gaps at the country level. Domestic antibiotic assessments should therefore integrate multiple data sources, including information on country-specific epidemiological profiles, procurement, sales volumes, and medicines management, among others, using a standard method. This aggregate information, presented in the form of national antibiotic assessment reports (NAARs), can successfully steer the formulation of national antibiotic policies. -
National antibiotic policies complement national action plans, facilitate access to antibiotics, and add accuracy to global target setting:
WHO recommended the creation of AMR NAPs in the early 2000s as a way for countries to identify concrete actions to address AMR. Within NAPs, domestic strategies on antibiotic use have generally focused on antibiotic stewardship at the patient level. In some cases, NAPs evolved into more comprehensive strategies geared towards strengthening surveillance and monitoring systems, improving infection prevention and control, and enhancing public awareness and education. IQVIA’s review of current NAPs indicated that only 35% of them reference antibiotic sourcing, funding, distribution, and responsible or rational use. In this regard, the formulation of national antibiotic policies, grounded in the data collected through NAARs, could allow countries to evolve their NAPs and gain more ownership in access. Based on this experience at the national level, international decision-makers could better understand the effectiveness of given interventions, and data generated by these domestic assessments could suggest what global usage and access targets should be. -
Data is essential for research and development, not only for the discovery of antibiotics but also vaccines:
High-quality datasets are also pivotal for the research and development of pharmacological solutions to fight AMR. Available tools are not only represented by many antibiotics but also by vaccines that can prevent multiple infections, reducing the risk of the use of anti-infectives and the potential emergence of resistance. At the same time, high-quality datasets are essential for demand forecasting, supporting the pharmaceutical industry in identifying unmet need before a product goes to market, and calibrating access considerations. -
Collecting reliable data requires increased investments in health system infrastructure:
Intelligence stemming from the medicine value chain—especially its discovery and access components—can also inform the investments necessary to create or maintain the health system infrastructure behind data collection. A study conducted by IQVIA and other partners in 14 African countries2 revealed that only 1.3% of the 50,000 laboratories in the sample conduct bacteriology testing, highlighting the urgency to improve diagnostic capacity as well as the workforce involved in it. Revamping laboratories in low- and middle-income countries is also a win-win situation as cross-cutting improvements benefit other disease areas and could also facilitate the rapid detection of potentially pandemic pathogens. To ensure the success of these interventions, AMR surveillance systems in laboratories and hospitals should design indicators that track patient readmissions and persistent infections to provide an early warning baseline. -
Ensuring access to antibiotics is a complex multi-stakeholder endeavor:
Getting the right antibiotics to the right place at the right time is not easy. From a pharmaceutical industry standpoint, relevant players in the field strive to bring medicines closer to those who need them by removing pricing barriers and contributing to other dimensions of the patient access pathway. Yet, the responsibility of ensuring access to antibiotics cannot be solely attributed to the private sector but shared with other players. Sustainable access is a joint endeavor that entails public-private partnerships with the potential to shape markets, accelerate health system transformations (particularly in diagnostics), and support the implementation of stronger stewardship protocols. This partnership approach becomes ever more relevant as health systems are confronting other emerging challenges, one of which is the displacement of AMR across geographies. It is not unlikely that resistant strains of diseases such as tuberculosis, to cite an example, could be crossing borders due to geopolitical conflicts and humanitarian crises, especially in high-burden countries in Eastern Europe. In such contexts, having the right data and cross-national partnerships can avert new infections effectively. -
Even though a lot still remains to be done, public-private partnerships are taking significant steps in the right direction:
Numerous organizations are serving as conduits for public and private investments meant to catalyze antibacterial innovation, step up diagnostics, and increase prevention. Many of these bodies are defined as public-private partnerships based on their diverse funding sources and the engagement of governments, the private sector, academia, and civil society in their governance processes and collaboration models. To encourage more research and development, these partnerships are leveraging the knowledge and capabilities of small- and medium-sized companies and many universities to devise new therapeutic solutions. While funding provided by these initiatives to researchers is a very important piece of the puzzle, the involvement of large pharmaceutical companies could provide guidance, expedite the discovery process, and assist first-class products in reaching the market.
The panel concluded by inviting relevant stakeholders to recognize their level and area of contribution and join partnerships that can realistically change the direction of travel of AMR. IQVIA will be focusing on the data-driven aspects of the response, hoping to lead the design and implementation of a collaborative approach that can support the realization of the 2024 AMR political declaration’s commitments.
1 Mora-Brito, D., Freeman, R., and Sharland, M. (2024). National ownership of antibiotic access and use: Driving policy decision-making based on population needs. IQVIA. https://shorturl.at/5BnGq
2 African Society for Laboratory Medicine (2024). MAAP country reports. https://aslm.org/what-we-do/maap/maap-country-reports/







