KEY POINTS
- Healthcare systems are under strain post-Covid, with 50-60% of EU&US HCPs reporting understaffing, resulting in substantial patient backlog.
- Enabling healthcare systems to deliver more efficient and effective care is at the heart of the pharmaceutical industry’s value proposition.
- Medical affairs teams play a key role by engaging effectively with stakeholders, understanding patient needs and providing timely and compelling evidence for the value of interventions.
- Pharma can learn from experiences in global health contexts, specifically from work done with challenged healthcare systems in low- and middle income countries – these learnings include
- Empowering patients transforms healthcare from a unilateral clinician decision to a two-way conversation makes a dramatic difference in effectiveness.
- Engagement with local stakeholders to avoid losing their expertise in the process.
- Focus on impact achieved, and choosing and tracking the right outcome metrics
DISCUSSION
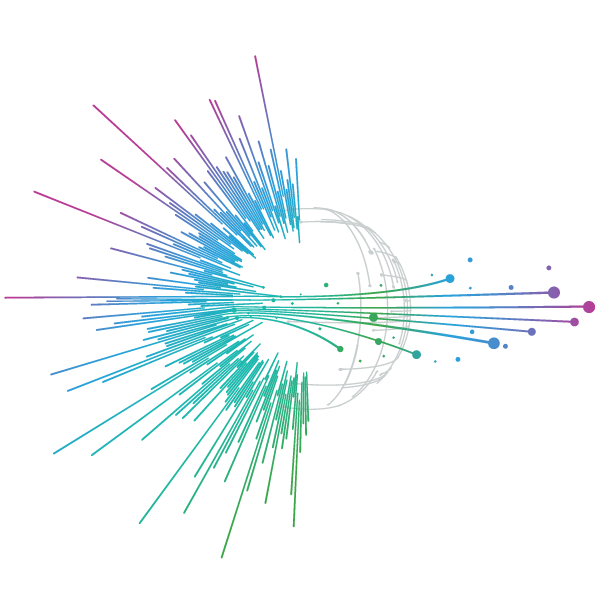
The ongoing pandemic has significantly amplified the strain on health systems worldwide, with the issue of understaffing becoming increasingly prevalent. In regions such as the EU and the US, understaffing rates hover around 60%, particularly in countries like Spain and the UK, resulting in substantial patient backlogs as highlighted in Figure 1. As a consequence, pharmaceutical and life sciences companies are seeking to integrate their products and services into the health care system, ensuring innovation that not only improves patient’s lives but also remove strain from the healthcare system.
Figure 1. Health system capacity gaps must be addressed to maximise the patient benefits of innovative treatments

Source: IQVIA EMEA Thought Leadership; 1. IQVIA Institute, Global Trends in R&D 2023: Activity, Productivity, and Enablers 2. IQVIA Primary Research, Impact of COVID-19 on Healthcare System in EU4, UK & US, March 2023
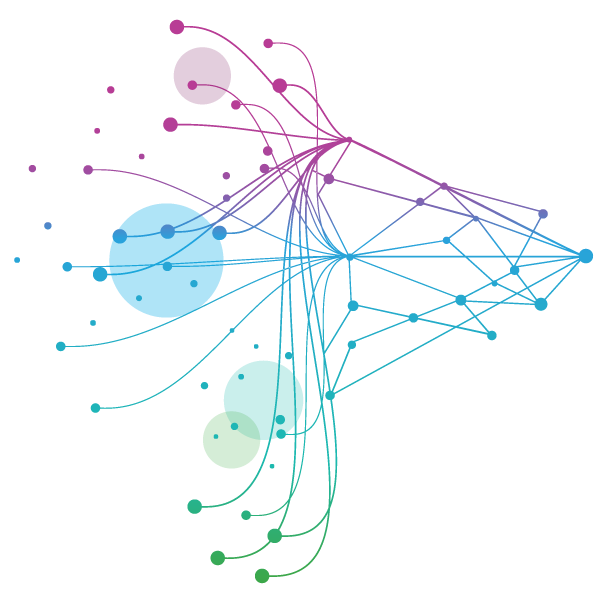
Competent medical affairs team, able to bridge these gaps with healthcare systems, are key in that endeavour. They are uniquely positioned to support health system capacity, provide timely and compelling evidence, and engage healthcare providers. A comprehensive understanding of the patient journey, from pre-diagnosis to treatment and outcomes, is essential, necessitating a holistic approach from medical affairs units as demonstrated in Figure 2.
Figure 2. Medical provides objectivity on barriers, data needs and drives KOL engagement to guide strategy

Source: IQVIA Analysis
Education and information play a central role in this process. Companies offering complex products need to engage with physicians, adopting an omnichannel approach that will undoubtedly rely heavily on face-to-face interactions. It is important to connect with physicians to comprehend the challenges they face and find effective solutions to address them.
Pharma engagement in Low- and Middle-Income Countries (LMICs) has always required a focus on healthcare systems enablement& transformation – so the questions that pharma teams must ask themselves on the impact of their solutions on the healthcare systems are very much alike while acknowledging that answers – and solutions will differ. While solutions for LMICs are often frugal compared to those in High-Income Countries (HICs), reflecting different funding allocations and a focus on population health versus efficiency, the approach to work with healthcare systems to enable efficient care is valid globally.
Enhancing patient understanding of their condition and treatments is critical and as an example can be encouraged by providing information sheets. This simple action can facilitate shared decision-making, transforming the process from a unilateral clinician decision to a two-way conversation which makes a dramatic difference in health provision effectiveness.
Data needs to be interpreted in a strategic and meaningful way, where the focus should be on generating data that illuminates unmet needs and provides insight into access and system effectiveness across systems. In regions like Africa where readily available data is scarce, many programs are often underpowered; this is where organisations like IQVIA can play a crucial role in providing the right data for decisions.
Partnerships should ideally be underpinned by clear theories of change with defined indicators and accountabilities. This is particularly relevant in global health, where stakeholders need to enhance their understanding considerably.
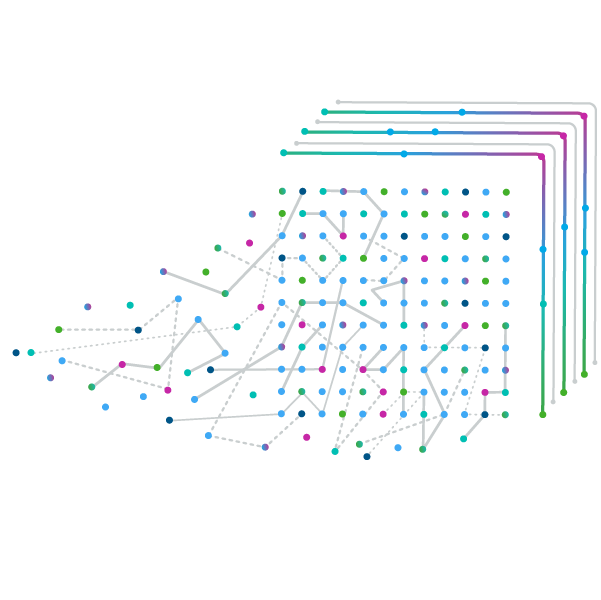
Lastly, while the U.S. benefits from extensive access to data and digitisation of medical records, the situation in Europe is less straightforward with variable implementation and attitudes towards digital health across member states. More work needs to be done globally to harmonise data standards, legislation, and access to technology.
Q&A
Why is data in LMICs important and what are the barriers in collecting it?
Data from LMICs is crucial as it offers a broader perspective on health and enables good decision-making. However, creating datasets and integrating them into disease intelligence poses challenges due to systemic gaps and lack of protocols. Furthermore, there is a good case for placing trials in regions like sub-Saharan Africa, given the increasing maturity of trial sites, trial metrics and rising diversity& inclusion requirements on clinical cohorts. The challenge lies in understanding how companies, particularly smaller ones, can engage effectively in this process without getting lost. Post-trial continuity and access will require a tailored
approach: how can efforts be sustained, and how can the rest of the value chain be established and maintained?
How to empower patients to make better decisions on their own health?
Patient involvement is crucial at every level, including the design of protocols. Medical affairs units should incorporate the patient's perspective, which can be facilitated through advocacy groups, patient organisations, and focus groups. Implementing a well-articulated programme can ensure this is a continuous process rather than a one-time occurrence. Increased patient engagement not only promotes a better understanding of their health but also enhances adherence to treatment, leading to improved health outcomes.
How can digitisation contribute to improve the patient journey?
Digitisation can significantly improve the patient journey, for example in epilepsy where diagnostics such as electroencephalograms (EEGs) are crucial. If these tools are not available in Primary Healthcare (PHC) settings, advanced digital tools can bridge this gap and enhance diagnostics.
The quality of patient outcomes is directly proportional to the robustness of PHC decisions. Digitisation can provide GPs with better information, particularly in cases where specialists are not available, thereby improving the patient journey. Similarly, digital tools can also support community health workers in LMICs, further strengthening global public health.
What are the skillsets required for success in medical affairs in the future?
The future of medical affairs necessitates a diverse range of skillsets. Professionals must be proactive and strategically-minded, with a deep understanding of challenges in the patient journey as well as market access considerations. Being collaborative is vital to improve interactions with commercial partners, and a business mindset is needed to identify company needs and investment areas. Additionally, many diseases come with patient stigmatisation. To change these beliefs, it is important to analyse behaviours and devise strategies for change, potentially involving sociologists or anthropologists.
The specific skillset required depends on the company's objectives. If the focus is on inclusive business models and addressing unmet needs, a thorough understanding of public health issues is crucial from an outside-in approach to see the bigger picture. Other important skills involve understanding patient access experience, understanding models of access to medicines in LMICs, and of course digital fluency in an increasingly tech-driven field.
NOTES
This article has been adapted from a panel discussion given by:
- Tim Wintermantel (Moderator), Sr. Principal, Global Public Health, IQVIA
- Michael Fürst, Global Head Social Business, UCB
- Nora Rösch, Global Medical Lead, Global Health Unit Sanofi
- David Kelaher, Sr. Dir. Medical Affairs, IQVIA
at the Switzerland Strategy Conference held in Basel on 7 February 2024